Contraception is defined as all methods voluntarily used by a person to prevent sexual intercourse from leading to a pregnancy. In addition, some of the methods presented below can also protect against STIs: sexually transmitted infections (condoms) or plan a pregnancy (natural methods).
CHARACTERITICS

It is not always easy to know which method is the best suit for you regarding contraception. Here are some characteristics specific to every contraceptive to inform and help you make a choice that fits your needs. Be aware that it is always possible to choose, change, ask questions, and discuss about it. Go to “Talk about it” page for further information.
CONTRACEPTIVE COMPATIBILITY

Contraception use is an important topic of discussion to have with your sexual partner.s. Indeed, there are no bad ways of managing fertility, as long as things are clear between partners. In this effect, it can be interesting to combine some contraceptives, either to increase the chance to avoid a pregnancy, to share the responsibility of contraception management, or even to avoid catching or transmitting sexually transmitted infections (STIs). The combined use of some methods can increase the effectiveness, but be aware, in other cases, it can also decrease the effectiveness! The table below indicates which methods can be used together or not. For any question, do not hesitate to talk about it to a doctor or a healthcare professional.
When should you take an emergency contraception?
Emergency contraception aims to prevent an egg and a sperm from meeting following sexual intercourse. Sperm can live for up to 5 days in the vagina and uterus. Emergency contraception works in different ways depending on the type:
- Emergency contraception in the form of a pill will act by delaying or inhibiting ovulation. It is no longer effective if fertilisation has occurred.
- Emergency contraception in the form of a copper IUD (coil) will cause a slight inflammatory reaction in the endometrium (inner lining of the uterus) due to the presence of its plastic structure, which prevents the implantation of a possible fertilised egg. Also, the copper wire in the IUD has a spermicidal reaction, i.e. it alters the motility (ability to move) of the sperm.
Other contraceptives use the same mechanisms of action, but are simply taken before sexual intercourse, while emergency contraceptives are taken following sexual intercourse. However, it should be noted that a fertilised egg that has already implanted in the endometrium constitutes a pregnancy. Emergency contraception has no impact on a pregnancy that has already started. If this is the case for you, please refer to the “unwanted pregnancy” page.
There are two main methods of emergency contraception:
There are many situations that can lead to the use of emergency contraception use. Refer to the table below for situations where there is a risk that your contraception may not have worked.
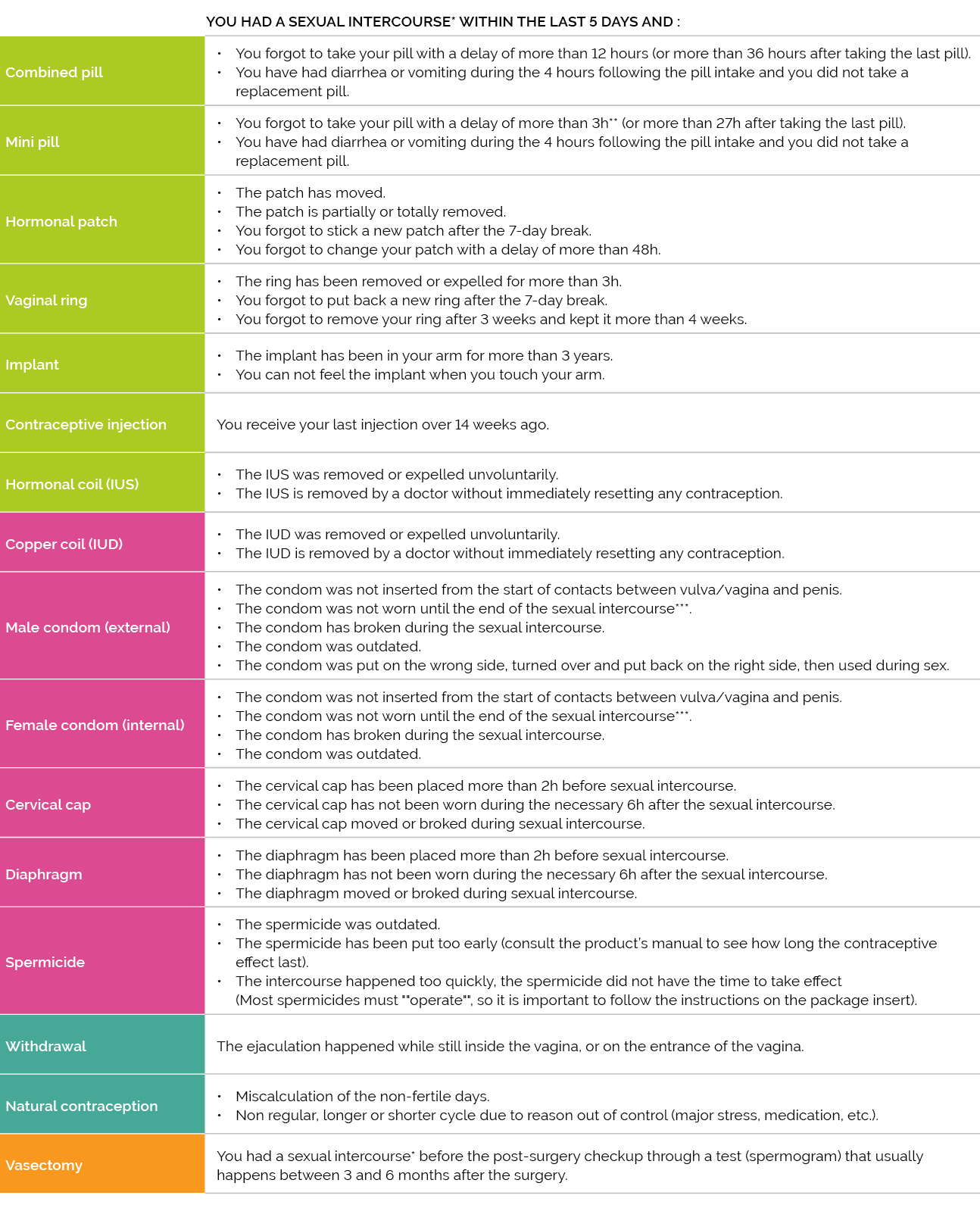
*Sexual intercourses without complementary contraception (e.g., no condom)
**attention, some mini pill made of desogestrel allow a delay up to 12 hours (or up to 36 hours after the intake of the last pill). Check the notice or ask your doctor/pharmacist.
***if your partner took of the condom without your consent and kept the penetration going without condom, the Penal Code and the jurisprudence in Luxembourg allows to assimilate this act to a rape or even to assault and battery in certain cases.
Frequently Asked Questions
Is withdrawal an effective method?
Withdrawal, also called “coitus interruptus”, consists of removing the penis from the vagina and surrounding area (vulva, anus) before ejaculation. The aim is to ensure that the semen does not come into contact with the vagina in order to minimise the risk of pregnancy. However, this method is not safe because the pre-seminal fluid (small amount of fluid secreted by the penis before ejaculation) may contain sperm. This means that the sperm may come into contact with the vagina or the entrance to the vagina. Even if there are fewer sperm in the pre-seminal fluid, fertilisation can happen. The effectiveness of this method depends on the partner’s ability to apply it proprely by withdrawing in time and avoiding ejaculating onto the vulva or into the vagina. It requires a great deal of control in a moment usually associated with “letting go”, which can make it difficult to apply properly in a systematic way. This method is therefore considered to be of low effectiveness when compared to other methods.
Note that withdrawal does not protect against sexually transmitted infections (STIs).
Can hormones cause blood clots?
First of all, taking contraception is a process that requires an appointment with a health professional. This process ensures that the health of the person requesting contraception is well protected.
Taking hormonal contraception, like any other medication, has some contraindications that your physician will review (e.g. smoking). Knowing your family health history may be useful.
A blood clot is a small mass of blood that can eventually block a blood vessel and prevent the flow of blood and oxygen to different parts of the body. Depending on where a blood clot is located, it is called a cardiovascular accident (brain), a phlebitis (legs) or a pulmonary embolism (lungs).
Here are some facts that help understand the risk of taking hormonal contraception :
- A woman not taking hormonal contraception: 1 to 10 women/10,000
- One woman taking the pill: 10-15 women/10,000
- A pregnant woman: 10-20 women/10,000
- A woman who has just given birth: 440 women/10,000
Taking hormonal contraception therefore slightly increases the risk of getting a blood clot, but these risks must be weighed against the benefits and, in any case, discussed with your physician!
Am I protected from pregnancy when I am breastfeeding?
Although the possibility is lower, pregnancy can occur during breastfeeding. When following a specific breastfeeding regime, the sucking of the breast by the newborn produces a hormone called prolactin. This hormone has the particularity of inducing a cessation of ovulation (anovulation). This breastfeeding can then be used as a temporary contraceptive method. This contraceptive method is called “LAM” for “lactation amenorrhea method”. In order to ensure its effectiveness, it is important to observe a few conditions thoroughly:
- No return of menstruation at all,
- The baby is less than 6 months old
- The baby is fed entirely on breast milk by sucking on the breast several times a day at strict and regular intervals.
It is possible to be helped and followed by a health professional for more information and guidance.
It is difficult to predict when ovulation will happen, and it may start as early as the first month after giving birth. It is therefore possible to get pregnant and advisable to always use another method of contraception while breastfeeding, even if it is exclusive. For more information on contraceptive methods that can be used following childbirth, you can refer to the following website: https://postpartumfp.srhr.org/.
Why is it called a pill generation?
The first-generation combined pill was developed in the 1950s. Since then, second, third and fourth generation pills have been developed. The generations of pills are differentiated according to the molecules they contain.
The third- and fourth-generation pills have recently been criticized for a slight increase of thrombosis risk compared to the second-generation pills. If you have any questions on this subject, please ask your physician, as there are several pills available.
I don't want to get my period again. Can I take an oestroprogestative contraceptive (combined pill, patch or vaginal ring) continuously for years?
There is no medical contraindication to taking the pill without a break to delay your period, but if you take the pill continuously for a longer period of time, there is a greater risk of having small irregular bleeding. (ref: https://pubmed.ncbi.nlm.nih.gov/25072731/)
Does hormonal contraception make you gain weight?
The first generations of pills were more heavily dosed than today: they sometimes caused very unpleasant side effects for women. Nowadays, during the first few cycles after starting the pill, women may notice a slight weight gain. On average, this can be up to 2 kilos. This weight gain can be explained by the oestrogens present in certain hormonal contraceptives, which can actually cause water retention. Be careful, weight gain can be explained in several ways, so you should be aware of all the possible causes of weight gain. If you have any questions or concerns, do not hesitate to consult your physician.
Isn't it easier not to use contraception and to take the emergency pill after having sexual intercourse?
The emergency pill is an emergency contraception, i.e. when the contraceptive method used to avoid pregnancy has not worked (e.g. forgotten pill, condom breakage, etc.) or when sexual intercourse occurred without any contraceptive method.
If you are in doubt about whether you need to take an emergency pill, don’t hesitate to talk to a health professional or a pharmacist. It is important to ask your questions as soon as possible, as the effectiveness of the emergency pill decreases with time. In other words, the longer you wait before taking the emergency pill, the less likely it is to work (maximum 3 to 5 days after the risky intercourse).
We use a male and a female condom at the same time. Clever, isn't it?
Unfortunately, not! There is a high risk that one of the two condoms will break. Choose the condom that suits you best.
How does the emergency pill work?
It delays ovulation through the action of progestin hormones. It should therefore be taken as soon as possible after unprotected sex.
Note: the emergency pill is not an abortion pill. This means that if the egg has already been fertilized, it may reduce the chances of implantation (implantation of the embryo in the lining of the uterus). On the other hand, if the embryo has already implanted in the endometrium, the emergency pill will have no effect, as the pregnancy has already begun.
This explains why the emergency pill is not 100% effective.
If you have recently used an emergency pill, it is highly recommended that you take a pregnancy test 19 days after taking the pill to check if it has worked.
Can the emergency pill be used frequently?
Some people use the emergency pill as a one-off contraceptive. It is not dangerous to use the emergency pill, even if it is taken more than once in a month. This is due to the composition of the pill, which contains only progestative. This synthetic hormone is not subject to any contraindication, which is why it can be purchased over the counter in pharmacies (no prescription is required). Side effects may occur after taking it, but usually disappear within 24 hours.
Note that the emergency pill does not protect against sexually transmitted infections (STIs). The emergency pill has no effect on unprotected sex following the intake. It is a “post-intercourse” contraceptive.
I take hormonal contraception. I used the emergency pill. Should I continue to take my hormonal contraception as usual?
The answer to this question depends on the type of emergency pill taken.
If you have taken the Norlevo© progestin-only pill (which can be taken up to 72 hours after unsafe sex), you must use a barrier method for the next 7 days (e.g. condom) AND continue to take your usual hormonal contraception as follows:
- If you are taking the mini-pill or combined pill, you can continue your pack as usual.
- If you use the patch, you must apply a new patch.
- If you use the vaginal ring, you must insert a new ring.
If you have taken the Ellaone© (Ulipristal acetate) pill (which can be taken up to 5 days after unsafe sex), you must use a barrier method and wait 6 days to resume your usual hormonal contraception. Once you have resumed hormonal contraception, you must wait for 7 days before having intercourse without a barrier method.
I have an emergency pill at home, and I am going to have unprotected sex, can I take it just beforehand for prevention?
No. The emergency pill must be taken after unprotected sex. If it is taken before, it will have no contraceptive effect (to prevent pregnancy).
Is it possible to stop having periods?
Some contraceptive methods can make periods disappear if taken continuously. This is the case with the hormonal IUD (intrauterine device), the implant and contraceptive injections.
With other contraceptive methods such as the pill, the patch or the vaginal ring, it is possible to delay period by one or more cycles. This can be discussed with your p
I have some bleeding outside my period. Is this normal?
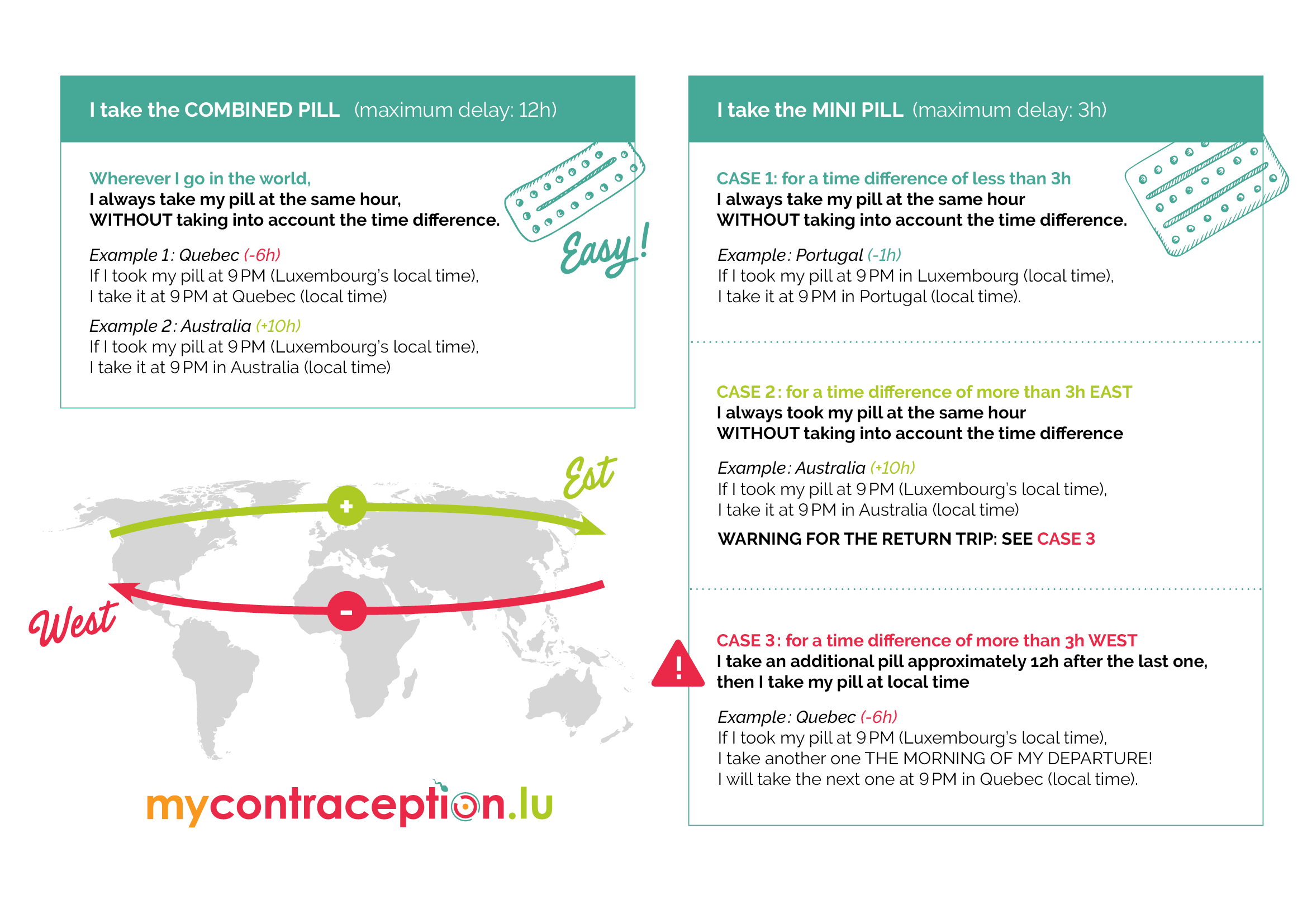
Bleeding outside the menstrual period can happen. Those bleedings are known as “spotting”. This bleeding is not usually serious or dangerous for your health and many women report having these symptoms whether or not they are using contraception. They are simply the result of a hormonal imbalance that can be caused by a change in hormonal contraception, an emotional change or great deal of stress, jet lag, having taken another month of hormonal contraception without a break, etc.
Bleeding at the time of ovulation is also possible and it is not dangerous.
If you are worried about bleeding happening outside of your period, don’t hesitate to talk to your physician.
If I have some bleeding outside of my period (spotting), should I stop my hormonal contraception for a few days?
No, you should not! If you stop using a hormonal contraceptive method (pill, patch, ring) for a few hours, it is possible that ovulation will occur! This will break your contraceptive cover. It is important to continue with your contraception as if nothing had happened, even if you have 2-3 days of spotting. If you are worried about spotting, do not hesitate to talk to your physician.
Can I smoke and take hormonal contraception?
Smoking is a contraindication to estrogenic hormonal contraception (combined pill, patch, vaginal ring) after the age of 35. Indeed, the natural ageing of the blood vessels combined with smoking and estrogen increases the risk of blood clots, responsible for cardiovascular accidents (brain), phlebitis (legs) or pulmonary embolisms (lungs). As a general rule, at the age of 35 onwards, smokers using estroprogestative contraception should consider other contraceptives to reduce these health risks.
Before the age of 35, it is possible to use estroprogestative contraception if you smoke, but the risk of a vessel complication is higher than if you did not smoke.
Do not hesitate to ask questions to your physician if you are in this situation: several alternatives exist!
What should I do if I forgot my pill?
If you forgot to take your pill, several things that should be considered: whether you had sex on the day you forgot or in the previous 5 days, the type of pill you are taking, during which week of the pack you forgot to take the pill, etc. It is best to refer to your pill leaflet or to a health professional.
You are no longer protected if you forgot to take the combined pill for more than 12 hours and if you forgot to take the mini-pill for more than 3 hours. Take the missed pill as soon as possible, even if this means taking the missed pill and the following one at the same time.
If you did not have sex on the day you forgot to take the pills and/or the previous 5 days, continue the pack, but use a condom for 7 days. You must take 7 consecutive-coloured pilles after you have missed a pill. If you come to the end of your pack after forgetting to take the pills, you should not take the white/placebo pills (see next question) but start a new pack directly. Please note that not all pills have placebo pills. If you do not have any white/placebo pills, continue your pack with no break.
If you had sex on the day you forgot to take the pill and/or in the previous 5 days, consult a health professional to find out what to do. If the intercourse took place recently, you can go to a pharmacy or Family Planning to take an emergency pill. While waiting for this emergency pill, continue to take the pill and if you have sex, use a condom. If it is the mini-pill and you have missed 2 or more pills, it is essential to contact your physician or a family planning centre to ask what to do. For the combined pill, if the missed pill is white/placebo, there is no consequences.
What is a placebo pill?
Placebo pills are a series of 7 pills (sometimes fewer), usually white (or different in colour from the hormone-containing pills). They are found in some combination pill packs that are used to maintain the habit of taking the pill every day during artificial menstruation (withdrawal bleeding*). There is no obligation to take these pills, but it is necessary to respect the number of days of withdrawal. Please note that the mini-pills (containing only progestative) do not have placebo pills.
* Bleeding, or withdrawal haemorrhage, is the monthly loss of blood when hormonal contraception is stopped. They are not “periods” in the same way as those that occur without hormonal contraception and are generally shorter.
Does hormonal contraception make my periods less painful and more regular?
Most hormonal contraceptives will result in a more predictable cycle, which may also be less painful. When you start taking hormonal contraception, however, irregular bleeding outside the period (spotting) may occur during the first few months.
What to do in case of an unwanted pregnancy?
In Luxembourg, each person has the freedom to choose, without constraint, whether or not to continue her pregnancy. Please note! Voluntary termination of pregnancy (VTP) is not a type of contraception. See the page “Unwanted pregnancy” for more information.
Is it possible to get pregnant from oral sex?
No. It is not possible to get pregnant from oral sex as the sperm does not come into contact with the entrance to the vagina.
However, oral sex without a condom does not protect against STIs.
Is pregnancy possible if there has been no penetration?
Yes, it is possible to get pregnant if the sperm has been in contact with the vulva/the entrance of the vagina and the sperm then travels up to the uterus. It is also important to know that sperm can also be present in the pre-seminal fluid (the small amount of fluid that lubricates the penis before ejaculation). In this case, there are fewer sperm, but they can still result in a pregnancy.
Sperm can also survive for up to 5 days after intercourse in the women’s internal genitalia, so there is a risk of pregnancy if the pill is missed within 5 days of intercourse.
It is also important to note that, for the same reasons, pregnancy can occur if using withdrawal method without an internal or external condom.
I had unprotected sex during my period, can I get pregnant?
If you are not using contraception, yes, it is possible to get pregnant if you have unprotected sex during your period. This is because sperm can survive in the women’s body for several days, and ovulation may occur in the days following your period.
If you are taking hormonal contraception, there is no risk of pregnancy, as long as you have taken your contraception properly.
Can a teenage girl get pregnant during her first few cycles and before her first period?
Yes, it is possible to get pregnant even before the first cycles arrive. In the menstrual cycle, ovulation occurs about 14 days before the period. So the first ovulation occurs about 14 days before the first period, and the egg can be fertilised at that time.
From the first ovulation, it is possible to become pregnant in every subsequent cycle if the person does not use contraception, until the menopause.
What contraception should I use if I regularly change sexual partners?
The best method of contraception is the one you choose to use and that suits you.
However, if you change sexual partners regularly, you should think about protecting yourself against sexually transmitted infections (STIs), for example by using barrier methods such as the internal or external condom or the dental dam, depending on the practice. Screening is also a way of being aware of your sexual health and protecting your partners as well.
Is it possible to combine several methods of contraception?
Yes, some contraceptives can be combined to increase their effectiveness. However, this is not the case for all contraceptives, and combining methods that are not meant to be combined can increase the risk of unwanted pregnancy.
For example, the external (male) condom and the internal (female) condom cannot be used at the same time, as this increases the risk of the condoms tearing.
On the other hand, the external or internal condom can be used at the same time as a hormonal method (pills, IUD, ring, patch, implant). In this way, contraception and protection against STIs are combined due to the condom.